TOTAL KNEE REPLACEMENT
If the knee is severely damaged by arthritis, injury or any reason, it will be hard for the patient to perform simple activities such as, walking, climbing stairs, bending or sitting. If nonsurgical treatments like medications are no longer helpful, that means the patient need total knee replacement surgery. Joint replacement surgery helps the patients to relieve pain and to do daily activities.
Anatomy
The knee is the largest joint in the body and it is made up of the lower end of the thighbone (femur), the upper end of the shinbone (tibia), and the kneecap (patella). The ends of these three bones are covered with articular cartilage. There are two menisci located between the femur and tibia. These C-shaped wedges act as "shock absorbers" that cushion the joint. In addition, there are four main ligaments (ACL, PCL, MCL, and LCL) within and around the knee.
Inside the knee, a thin lining called the synovial membrane surrounds the joint. This membrane releases a fluid that feeds the cartilage, some part of menisci and reduces friction.
Causes
The most common cause of chronic knee pain and disability is arthritis. Although there are many types of arthritis, most knee pain is caused by just three types: osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis.
Osteoarthritis
Osteoarthritis is the most common form of arthritis in the knee. It is a degenerative, wear-and-tear type of arthritis that occurs most often in people 50 years of age and older. In osteoarthritis, the cartilage in the knee joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone, and produce painful bone spurs. Osteoarthritis develops slowly and the pain it causes worsens over time.
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic autoimmune disease (immune system attacks its own tissues) that attacks multiple joints throughout the body. The immune system damages normal tissue (such as cartilage and ligaments) and softens the cartilage. This chronic inflammation damages the cartilage and eventually cause cartilage loss, pain, and stiffness.
Posttraumatic Arthritis
Posttraumatic arthritis develops after a serious knee injury. For example, a broken bone of the tibia, the femur or the patella may damage the joint surface and lead to arthritis years after the injury. In addition, the torn meniscus and ligament injuries can cause instability and additional wear on the knee joint, which over time can result in arthritis.
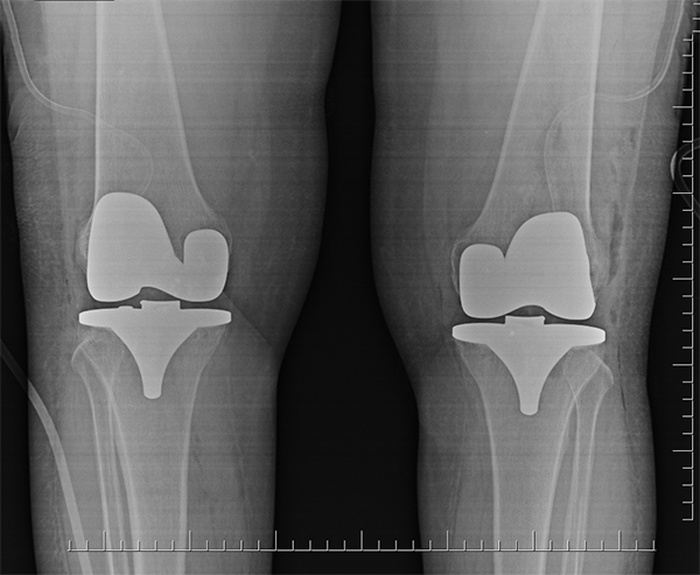
Description
The knee replacement (arthroplasty) means to change the damaged surface of the joint with metallic implants. There are three basic steps to a knee replacement procedure: First the damaged cartilage surface of the femur and the tibia (Sometimes patella) are removed and the bones are prepared. Second the femur and the tibia metal components are placed in appropriate position with cement or without cement (pres- fit). Finally a medical-grade plastic spacer is inserted between the metal components of tibia and femur.
When Surgery Is Recommended
People who benefit from total knee replacement are as follows:
- When the patient has severe knee pain or stiffness that limits daily activities, such as walking, climbing stairs.
- When the pain does not improve with other treatments such as anti-inflammatory medications, cortisone injections, lubricating injections and physical therapy.
- When chronic knee inflammation and swelling that does not improve with rest or medications.
There are no absolute age or weight restrictions for total knee replacement surgery. Recommendations for surgery are based on a patient's pain and disability.
The Orthopaedic Evaluation
The orthopedics surgeon check the patient gets his/her medical history and needs some imagings (X-Ray, MRI) and laboratory tests to decide about the treatment and plan about the operation.In addition, the orthopaedic surgeon will explain the potential risks and complications of total knee replacement, including those related to the surgery itself and those that can occur over time after the surgery.
Surgical Procedure
First the damaged cartilage surface of the femur and the tibia (Sometimes patella) are removed and the bones are prepared. Second the femur and the tibia metal components are placed in appropriate position with cement or without cement (pres- fit). Finally a medical-grade plastic spacer is inserted between the metal components of tibia and femur.
What is Knee Replacement?
The knee replacement (arthroplasty) means to change the damaged surface of the joint with metallic implants. There are three basic steps to a knee replacement procedure: First the damaged cartilage surface of the femur and the tibia (Sometimes patella) are removed and the bones are prepared. Second the femur and the tibia metal components are placed in appropriate position with cement or without cement (pres- fit). Finally a medical-grade plastic spacer is inserted between the metal components of tibia and femur.
Possible Complications of Surgery
The complication rate following total knee replacement is low. Serious complications, such as a knee joint infection, blood clots, implant problems, continued pain and neurovascular injury are less than 2%.
Infection: Infection may occur in the wound or deep around the prosthesis. Minor infections in the wound area are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the prosthesis.
Blood clots: Blood clots in the leg veins are a common complication of knee replacement surgery. Blood clots can form in the deep veins of the legs or pelvis after surgery. To prevent blood clot the patient should do periodic elevation of the legs, lower leg exercises to increase circulation, support stockings, and blood thinners such as warfarin (Coumadin), low-molecular-weight heparin, and aspirin can help prevent this problem.
Implant problems: Although implant designs and materials continue to advance, implant surfaces may wear down and the components may loosen.
Continued pain: A small number of patients continue to have pain after a knee replacement. This complication is rare.
Neurovascular injury: While rare, injury to the nerves or blood vessels around the knee can occur during surgery.
Physical Therapy
Most patients can begin exercising their knee hours after surgery. The doctor will teach the patient specific exercises to strengthen the leg and restore knee movement to allow walking and other normal daily activities soon after the surgery.
Activity
Exercise is a critical component of home care, particularly during the first few weeks after surgery. The patient should be able to resume most normal activities of daily living within 3 to 6 weeks following surgery.
© COPYRIGHT 2025 ALL RIGHTS RESERVED
Privacy Policy